Muscle Contraction or Signal Failure?
- vucuthocasi
- Jul 6, 2025
- 3 min read

Muscle Contraction or Signal Failure?
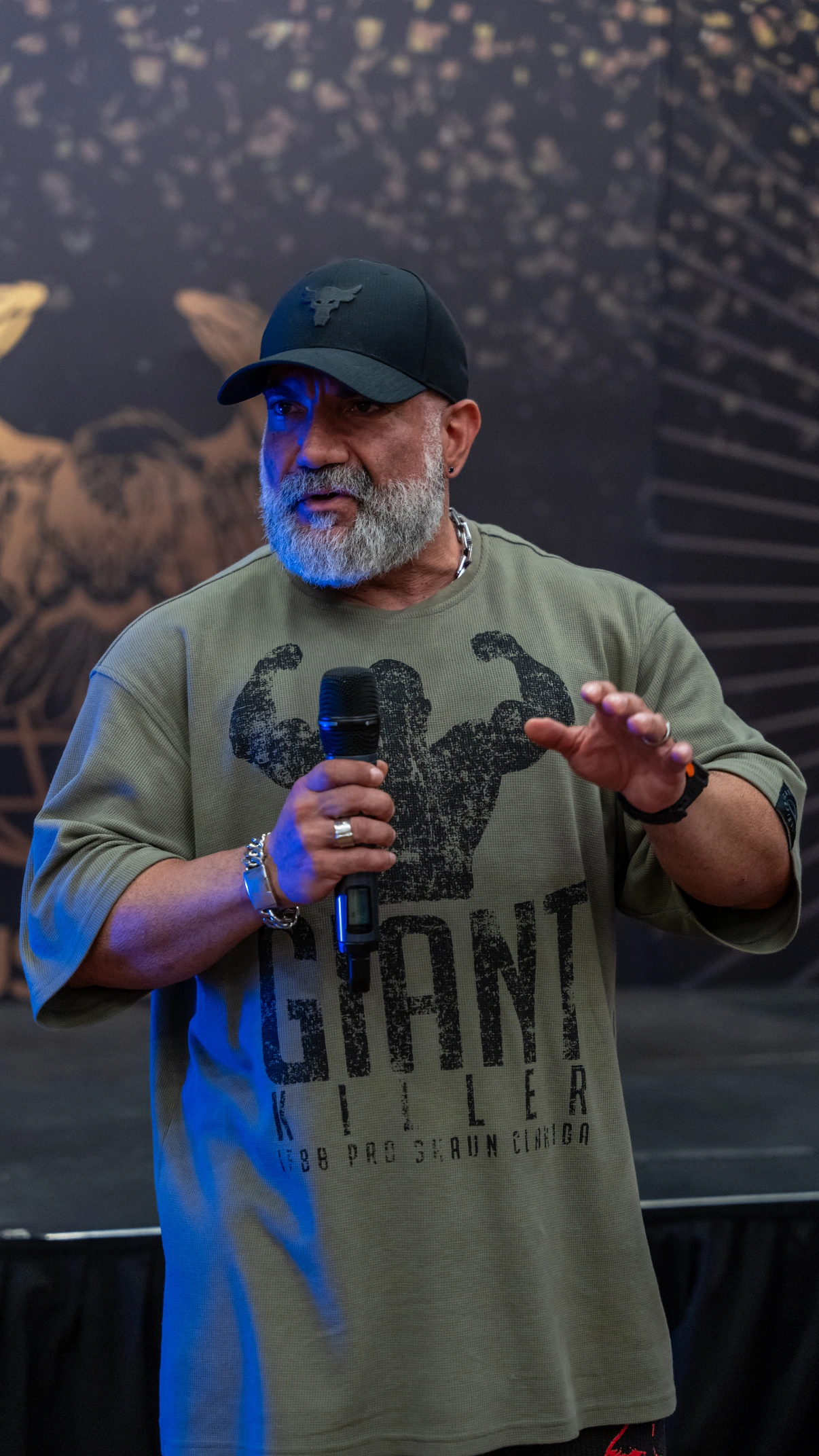
Written by: IFBB PRO COACH CAN ÜNAL
Prolonged and severe muscle cramps often carry critical physiological signals. Whether you're chasing peak performance or protecting long-term health, interpreting these signs accurately is essential. In this article, we delve into each root cause and mechanism, supported by scientific evidence.
1. Disruption in Neuromuscular Transmission
Muscles don’t act independently; they respond to commands from the nervous system. If this communication line is compromised, involuntary and prolonged contractions—i.e., cramps—are inevitable.
A) Hyperexcitable Neural Stimulus
Under fatigue, stress, or overstimulation, the central nervous system may fire motor neurons uncontrollably, causing sustained contraction and difficulty in relaxation.
B) Nocturnal Cramps
Cramps during sleep are common, especially in older adults. They are linked to increased neuromuscular excitability during rest, where the inhibitory mechanisms of the nervous system become less effective.
C) Motor Neuron Imbalance
Certain neurological conditions disrupt the excitation-inhibition balance of motor neurons, leading to spontaneous and prolonged muscle contractions.
2. Electrolyte Imbalance
Muscle function relies on the precise balance of ions such as Na⁺, K⁺, Ca²⁺, and Mg²⁺. These ions regulate membrane potential and neuromuscular transmission.
A) Potassium (K⁺) Deficiency
When potassium balance is disrupted, neuromuscular hyperexcitability occurs. Hypokalemia (K⁺ < 3.5 mmol/L) increases the risk of cramps and muscle weakness.🔗 Hypokalemia – Wikipedia
B) Calcium and Magnesium Balance
Calcium supports contraction, while magnesium enables relaxation. Magnesium deficiency compromises ATP production and decreases relaxation efficiency.🔗 Magnesium & Cramp – PMC
A study in pregnant women found a significant correlation between low magnesium levels and cramping (p=0.000), while calcium and potassium showed no such association.🔗 ResearchGate Article
C) Fluid-Electrolyte Depletion
Intense training leads to excessive Na⁺ and Cl⁻ loss via sweat. If not replenished properly, interstitial pressure rises and motor nerves are compressed, increasing cramp susceptibility.
3. Overtraining and Muscular Fatigue
Muscles, like neurons, require adequate recovery. When overused, their energy balance is disrupted, leading to spasms and cramping.
A) Lactic Acid Accumulation
During anaerobic metabolism, lactic acid builds up, lowering intramuscular pH and promoting involuntary contractions.
B) Overloaded Type 2 Fibers
Heavy resistance training recruits Type 2 fibers, which—when fatigued—impair neuromuscular feedback loops, resulting in spontaneous spasms.
C) Glycogen Depletion and Recovery Failure
Inadequate glycogen replenishment weakens neuromuscular signaling and prolongs contraction duration due to reduced ATP availability.
4. Insufficient Warm-Up and Lack of Stretching
Muscles need time and movement to prepare for exertion. Without proper preparation, they become mechanically and neurologically vulnerable.
A) Sudden Contraction in Cold Muscles
Unwarmed muscles are less elastic and more prone to injury and spasm upon sudden exertion.
B) Lack of Static Stretching
Pre- and post-training static stretches stabilize muscle tone and reduce stretch reflexes, decreasing cramp incidence.
C) Postural Imbalances and Asymmetry
Uneven loading on muscle groups leads to localized stress, particularly in the lower back, glutes, and calves—frequent cramp zones.
5. Circulatory Deficiencies
If oxygen and nutrients don’t adequately reach muscle cells, fatigue sets in rapidly, followed by cramping.
A) Varicose Veins and Venous Insufficiency
Poor circulation in the lower limbs results in oxygen-deficient muscle tissue, prolonging contraction and increasing cramp risk.
B) Deep Vein Thrombosis (DVT)
A clot impairs blood flow and may compress surrounding nerves, triggering involuntary contractions.
C) Compartment Syndromes
When fascial pressure increases, nerves and vessels become compressed, causing localized, prolonged cramps.
6. Medications and Systemic Disorders
Certain medications and diseases can alter neuromuscular function or electrolyte balance, directly contributing to cramping.
A) Diuretics, Statins, and Beta-Agonists
These drug classes can cause electrolyte disturbances or impair nerve-muscle communication.🔗 Practical Neurology: Muscle Cramps
B) Statins
May cause microscopic damage to muscle fibers, lowering the cramp threshold.
C) Hypothyroidism and Diabetic Neuropathy
In hypothyroidism, slowed metabolism impacts muscle contraction cycles. In diabetes, nerve damage increases spontaneous cramping.
Scientific Parameters & Reference Ranges
Parameter | Normal Range | Relevance to Cramps |
Serum K⁺ | 3.5–5.0 mmol/L | <3.5: Hypokalemia → cramps, weakness |
Serum Mg²⁺ | 0.70–1.10 mmol/L | <0.70: Hypomagnesemia → spasm, ATP dysfunction |
Serum Ca²⁺ | 8.5–10.5 mg/dL | Imbalance impairs contraction/relaxation cycle |
Sweat Na⁺ Loss | >2.3 g/hour (heavy loss) | Risk factor for exercise-associated muscle cramps (EAMC) |
Suggested Scientific Sources
🔗 Practical Neurology on Drug-Induced Cramps
Conclusion: A Cramp Is Not Just a Feeling — It's a Signal
Prolonged cramps are not random; they are messages from your body demanding attention. Whether you're an athlete or sedentary, understanding these signs is key to optimizing performance and preserving health. Respect your muscles, and they will perform accordingly.
.png)



Comments